“I didn’t want my picture taken because I was going to cry. I didn’t know why I was going to cry, but I knew that if anybody spoke to me or looked at me too closely the tears would fly out of my eyes and the sobs would fly out of my throat and I’d cry for a week. I could feel the tears brimming and sloshing in me like water in a glass that is unsteady and too full.” - Sylvia Plath
Nothing among the stack of books or reading materials from my initial breast cancer diagnosis reflects my current state of being. This stage IV cancer is not "crazy sexy;" I'm not feeling like a badass; I haven't been able to heal by hoping for it; and I cannot stomach tea or coffee while on my current treatments.
Breast cancer has become so pink-washed by our society that most of us only think about the beatable, survivable stuff. The chemo-surgery-radiation cycle responsive breast cancer.
I don't have that. I have the kind of cancer that kills women within an average of 3 years and is wildly under-researched (see https://www.youtube.com/watch?v=FpSu9U1yXA0). Metastatic AND triple negative breast cancer is ugly stuff.
More immediately, I have the kind of cancer that really hurts. It's physically painful to sit, lay, stand, etc. I didn't know about this! My lungs, with their pleural effusions (the fluid in the lining around my lungs), hurt badly. Like rolling-in-bed-moaning-tearfully badly. Some of my bones where cancer has taken up residence feel as though knives are being scraped along them. My back constantly hurts. When I cough from the cancer nodules in my lungs and lymphatics, my whole body shakes and aches. Sleep is not restful... no matter how long I lay there and even knock off, the fatigue doesn't go away.
All of this - and more - has contributed greatly in the past month to me feeling depressed. Seriously in a funk of the clinical sort.
Some of you have noticed. Thank you for reaching out and for understanding the radio silence you've received in return. Your cards, calls/voicemails, texts, Facebook messages, and more are appreciated. I just don't always know what to say or how to muster the energy sometimes to respond.
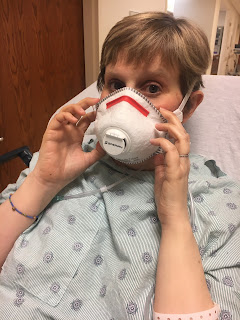
 |
| All decked out in cords and monitors for my hospital stay |
Meanwhile, the pulmonary doctors at Northwestern were very concerned about how quickly my right lung was accumulating fluid. So, on Tuesday, I had to get a second catheter/drain - this time on the right side where fluid is building up. Sean has to drain that side daily, and we're still getting out more fluid than we'd like.
We spent the remainder of that week at my parents’ house, where I could barely get out of bed and couldn't eat much of anything. We drove back to Colorado (via the much shorter northern route) over the weekend. It was still a long, painful ride for me.
By the time we arrived home, my depression was full-blown. The pain, the isolation, the seemingly endless string of health issues to endure... it wiped me out. I'm physically weak, struggling to eat even small meals, crying a lot, and requiring loads of help to do even basic tasks. Oh, and the oxygen tanks. Nothing makes you feel prematurely on your deathbed like having to wear a nasal cannula and lug around tanks of oxygen. When I'm at home and hooked up to the oxygen compressor, I have 50 feet of cord trailing me. We were able to get a portable compressor this week for travel purposes, which will make flying on planes possible again.
And, since I told you that my type and stage of breast cancer is nasty, I'll share one more bombshell. Remember that vision change I mentioned I was experiencing a few posts ago? Well, the Northwestern team wanted me to get a brain scan to check that out. I spent a peaceful 30 minutes in prayer and thanking God for all His gifts while the MRI machine rattled and banged around me. Unfortunately, those results came back last night, and there is a 3mm cancerous lesion on my brain.
I'm officially on the treat-scan-repeat path now. The spot on my brain is treatable with targeted radiation, but next steps will depend on what the Northwestern clinical trial team decides to do with me. It's possible that this brain metastasis could make me ineligible for the immunotherapy trial I'm on. The decisions lie in their hands.
So, there it is. Your prayers and thoughts would be very much appreciated. Still hoping for miracles and a full cure, but feeling God may have other plans for me. Our hearts, minds, emotions, and bodies need strength and patience and peace. We pray for the doctors at Northwestern to make good decisions about my care, and we pray for us and our families to receive the support we need.
“I have told you these things, so that in me you may have peace. In this world you will have trouble. But take heart! I have overcome the world.” - John 16:33